


Treatment of toxic overdose include a short-acting barbiturate or diazepam to treat excitement and convulsions. Severe overdose may result in circulatory collapse, respiratory failure, paralysis, and coma. Toxic doses can cause palpitations, restlessness, hallucinations, delirium, and coma. The following symptoms could signal overdose: palpitations, dilated pupils, difficulty swallowing, hot dry skin, thirst, dizziness, restlessness, tremor, fatigue, and ataxia. The action of atropine may be enhanced by tricyclic antidepressants, monoamine oxidase inhibitors (MAOI’s), phenothiazine, amantadine, some antihistamines, butyrophenones, and disopyramide.
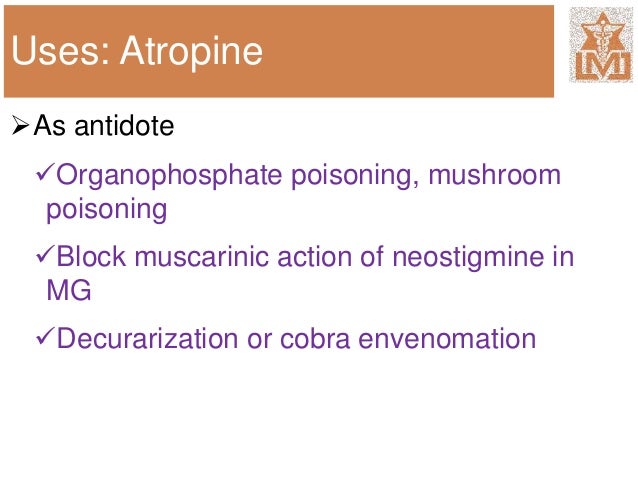
Pyloric stenosis: atropine may cause complete obstruction.Suspected glaucoma: atropine may precipitate acute glaucoma.Consult the complete product insert for pediatric dosing.Ĭommon side effects of atropine include dry mouth, blurred vision, photophobia, tachycardia, flushed skin, constipation, difficulty with urination, inability to perspire appropriately, delirium or coma (McLendon & Preuss, 2021).Ītropine may cause adverse effects in patients with the following conditions: Note: The safety and efficacy of atropine in pediatric patients has not been fully studied. Severe symptoms: 3 to 5 mg IV bolus and repeat as above consider IV continuous infusion.Mild to Moderate symptoms: 1 to 2 mg IV bolus repeat by doubling the dose every 3 to 5 minutes if previous dose did not induce a response repeat doses as needed for 2 to 12 hours for recurrence of symptoms consider starting IV continuous infusion for improved clinical outcomes.1 to 2 mg IV titrate and repeat as needed to reverse symptoms (i.e., titrate to decreased bronchial secretions)Īntidote for anticholinesterase poisoning (carbamate insecticides, nerve agents, organophosphate insecticides).Treatment of symptoms from muscarine-containing mushroom poisoning 0.5 to 1 mg IM, IV or subcutaneously 30 to 60 minutes preoperatively repeat very 4 to 6 hours as needed.

Preoperative/preanesthetic medication to inhibit salivation and secretion Endotracheal: 1 to 2 mg every 3 to 5 minutes.1 mg is preferred for severe bradyarrhythmias (i.e., hypotension/shock, altered mental status, acute heart failure).0.5 to 1 mg IV or IM every 3 to 5 minutes.15 to 20 mcg/kg IV when administered with neostigmine.5 to 7 mcg/kg IV when administered with edrophonium.Atropine Sulfateīradycardia during neuromuscular blockade reversal For ET administration, dilute 1 mg to 2 mg in 10 mL of sterile water or normal saline (McLendon & Preuss, 2021). Atropine may be administered subcutaneously, intramuscularly (IM), intravenously (IV), intraosseous, or by endotracheal tube (ET). It is a competitive, reversible antagonist of muscarinic receptors and can be used to reverse the muscarinic effects of cholinergic poisoning (Lexicomp, n.d.). Atropine blocks the action of acetylcholine at parasympathetic sites in smooth muscle, secretory glands, and the central nervous system, which leads to increased cardiac output and dries secretions. Facing Ethical Challenges with Strength and CompassionĪtropine is an anticholinergic drug.
#Atropine antidote neostigmine professional#
Establishing Yourself as a Professional and Developing Leadership Skills.Ensuring Patient & Family Centered Care.Developing Critical Thinking Skills and Fostering Clinical Judgement.Alteplase Injection for Acute Ischemic Events.Affirming Care for Patients who are LGBTQ+.Lippincott Clinical Conferences On Demand.Continuing Education Bundle for Nurse Educators.Lippincott NursingCenter’s Critical Care Insider.Lippincott NursingCenter’s Career Advisor.An Unforeseen Path from Critical Care Nurse to Editor-in-Chief of American Journal of Nursing.When Nurses Speak, People Listen: An Interview with Pat Patton.Academic/Practice Innovation: An Interview with Dr.Nurse Wellness Is Not Just About Resiliency.Creating Learning Environments to Advance Health Equity.Using Simulation to Develop Clinical Reasoning.The Nursing Shortage and Nurse/Patient Ratios.


 0 kommentar(er)
0 kommentar(er)
